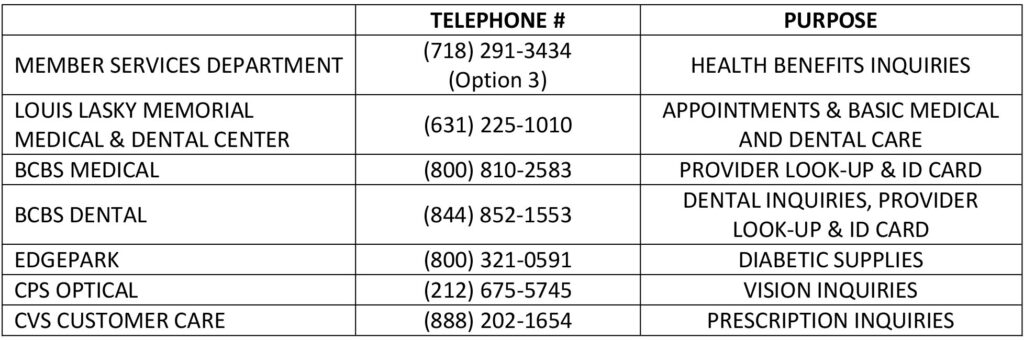
List of Important Phone Numbers
Frequently Asked Questions Regarding Your Health Benefits
For assistance in reviewing the EOB you received, please contact the Member Services Department.
For optical benefits, refund reimbursement, or participating providers, contact Comprehensive Professional System (CPS), Inc. at 212-675-5745 or www.cpsoptical.com for provider look-up and additional information concerning your optical benefits.
For dental information, contact Blue Cross dental customer service at 844-852-1553.
Chiropractic services for children is not a covered benefit.
Acupuncture is not a covered benefit.
Reimbursement for Gym membership is not a covered benefit.
Contact Employer Services Department at 718-291-3434 and request to speak with a representative.
For change in marital status or birth of a child, contact the Employer Services Department and provide a copy of the document (divorce decree, birth certificate, etc.).
Call the Member Services Department at 718-291-3434 (option 3) to discuss the specifics of your situation.
For a listing of participating providers, you can:
- Call Anthem at 800-810-2583
- Visit the Anthem website empireblue.com/find-care/; or
- Call the Member Services Department at 718-291-3434 (option 3).
Prescription-related problems are typically caused by one or more of the factors listed below; for assistance in resolving these issues, contact the Member Services Department.
- Incorrect patient identification number
- Incorrect date of birth
- No Prior Authorization (PA) on file
- Non-covered services
- Medication has a quantity limit
- Check the Blue Cross website https://bcbsglobalcore.com for a listing of participating providers
- To obtain medical assistance or provider information, contact 1-800-810-BLUE or call collect at 1-804-673-1177
Immediately contact the Member Services Department, legibly complete and sign the forms to prevent delay in claims processing.
Request the procedure codes from your doctor’s office and contact the Member Services Department to verify if the treatment is a covered service and if precertification is required.
Contact Member Services at the number listed on the back of your insurance id card and make sure to have your paperwork or date of service you are referencing.
Contact the Member Services Department to inquire why the claim was denied and if necessary, you can request to appeal in writing. Please see Section 6.6 of the General and Administrative Section of your Summary Plan Description for further information regarding how to appeal further.
- Seek medical attention, if necessary.
- Immediately report the incident to your supervisor.
- Provide your employer’s telephone number, address or, if known, workers’ compensation insurance (NOT your medical insurance) carrier information to all medical personnel treating your injury.
- Seek medical attention, if necessary.
- Immediately report the accident to your No-Fault Insurance carrier.
- Provide your No-Fault Insurance (NOT your medical insurance) carrier information to all medical personnel treating your injury.
